Everything you need to know about COVID-19 vaccines.
Tetra/Getty
For the most up-to-date news and information about the coronavirus pandemic, visit the WHO website.
COVID-19, the potentially fatal respiratory illness first detected in December 2019, has spread across the globe with unseen speed and ferocity. It’s forced the cancellation of major events, postponed sports seasons, and sent the world into self-isolation in an attempt to curb the spread. Health authorities and governments are attempting to flatten the curve and mitigate extensive transmission in the community, while biotech firms and researchers turn their attention to the coronavirus causing the disease: SARS-CoV-2.
Since it was first discovered as the causative agent of the new disease, scientists have been racing to get a better understanding of the virus’ genetic makeup, how it infects cells and how to effectively treat it. There’s no cure, and medical specialists can only treat the symptoms of the disease. Many different treatment options have been proposed and some older drugs seem to be associated with positive outcomes — but much more work is required. However, the long-term strategy to combat COVID-19, which has spread to every continent on Earth besides Antarctica, is to develop a vaccine.
Developing new vaccines takes time, and they must be rigorously tested and confirmed safe via clinical trials before they can be routinely used in humans. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases in the US, has frequently stated that a vaccine is at least a year to 18 months away. Experts agree there’s a ways to go yet.
Vaccines are incredibly important in the fight against disease. We’ve been able to keep a handful of viral diseases at bay for decades because of vaccine development. Even so, there exists confusion and unease about their usefulness. This guide explains what vaccines are, why they are so important and how scientists will use them in the fight against the coronavirus. It also discusses the current treatment options being used and those that show promise in hospitals.
As more candidates appear and are tested, we’ll add them to this list, so bookmark this page and check back for the latest updates.
You can jump to any segment by clicking the links below:
- What is a vaccine?
- What’s in a vaccine?
- Making a COVID-19 vaccine
- When will a vaccine be available?
- First COVID-19 vaccine trials in the US
- How do you treat COVID-19?
- The trouble with chloroquine
- Convalescent plasma therapy
- How you can protect yourself from coronavirus now
What is a vaccine?
A vaccine is a type of treatment aimed at stimulating the body’s immune system to fight against infectious pathogens, like bacteria and viruses. They are, according to the World Health Organization, “one of the most effective ways to prevent diseases.”
The human body is particularly resilient to disease, having evolved a natural defense system against nasty disease-causing microorganisms like bacteria and viruses. The defense system — our immune system — is composed of different types of white blood cells that can detect and destroy foreign invaders. Some gobble up bacteria, some produce antibodies which can tell the body what to destroy and take out the germs, and other cells memorize what the invaders look like, so the body can respond quickly if they invade again.
Vaccines are a really clever fake-out. They make the body think it’s infected so it stimulates this immune response. For instance, the measles vaccine tricks the body into thinking it has measles. When you are vaccinated for measles, your body generates a record of the measles virus. If you come into contact with it in the future, the body’s immune system is primed and ready to beat it back before you can get sick.
The very first vaccine was developed by a scientist named Edward Jenner in the late 18th century. In a famous experiment, Jenner scraped pus from a milkmaid with cowpox — a type of virus that causes disease mostly in cows and is very similar to the smallpox virus — and introduced the pus into a young boy. The young boy became a little ill and had a mild case of cowpox. Later, Jenner inoculated the boy with smallpox, but he didn’t get sick. Jenner’s first injection of cowpox pus trained the boy’s body to recognize the cowpox virus and, because it’s so similar to smallpox, the young man was able to fight it off and not get sick.
Vaccines have come an incredibly long way since 1796. Scientists certainly don’t inject pus from patients into other patients, and vaccines must abide by strict safety regulations, multiple rounds of clinical testing and strong governmental guidelines before they can be adopted for widespread use.
What’s in a vaccine?
Vaccines contain a handful of different ingredients depending on their type and how they aim to generate an immune response. However, there’s some commonality between them all.
The most important ingredient is the antigen. This is the part of the vaccine the body can recognize as foreign. Depending on the type of vaccine, an antigen could be molecules from viruses like a strand of DNA or a protein. It could instead be weakened versions of live viruses. For instance, the measles vaccine contains a weakened version of the measles virus. When a patient receives the measles vaccine, their immune system recognizes a protein present on the measles virus and learns to fight it off.
A second important ingredient is the adjuvant. An adjuvant works to amplify the immune response to an antigen. Whether a vaccine contains an adjuvant depends on the type of vaccine it is.
Some vaccines used to be stored in vials that could be used multiple times and, as such, contained preservatives that ensured they would be able to sit on a shelf without growing other nasty bacteria inside them. One such preservative is thimerosal, which has garnered a lot of attention because it contains trace amounts of easily cleared ethylmercury. Its inclusion in vaccines hasn’t been shown to cause harm, according to the CDC. In places like Australia, single-use vials are now common, and thus preservatives such as thimerosal are no longer necessary in most vaccines.
In developing a vaccine for SARS-CoV-2, scientists need to find a viable antigen that will stimulate the body’s immune system into defending against infection.
Making a COVID-19 vaccine
The pathogen at the center of the outbreak, SARS-CoV-2, belongs to the family of viruses known as coronaviruses. This family is so named because, under a microscope, they appear with crownlike projections on their surface.
In developing a vaccine that targets SARS-CoV-2, scientists are looking at these projections intensely. The projections enable the virus to enter human cells where it can replicate and make copies of itself. They’re known as “spike proteins” or “S” proteins. Researchers have been able to map the projections in 3D, and research suggests they could be a viable antigen in any coronavirus vaccine.
That’s because the S protein is prevalent in coronaviruses we’ve battled in the past — including the one that caused the SARS outbreak in China in 2002-03. This has given researchers a head start on building vaccines against part of the S protein and, using animal models, they’ve demonstrated they can generate an immune response.
There are many companies across the world working on a SARS-CoV-2 vaccine, developing different ways to stimulate the immune system. Some of the most talked about approaches are those using a relatively novel type of vaccine known as a “nucleic acid vaccine.” These vaccines are essentially programmable, containing a small piece of genetic code to act as the antigen.
Biotech companies like Moderna have been able to generate new vaccine designs against SARS-CoV-2 rapidly by taking a piece of the genetic code for the S protein and fusing it with fatty nanoparticles that can be injected into the body. Imperial College London is designing a similar vaccine using coronavirus RNA — its genetic code. Pennsylvania biotech company Inovio is generating strands of DNA it hopes will stimulate an immune response. Although these kinds of vaccines can be created quickly, none have been brought to market yet.
Johnson & Johnson and French pharmaceutical giant Sanofi are both working with the US Biomedical Advanced Research and Development Authority to develop vaccines of their own. Sanofi’s plan is to mix coronavirus DNA with genetic material from a harmless virus, whereas Johnson & Johnson will attempt to deactivate SARS-CoV-2, essentially switching off its ability to cause illness while ensuring it still stimulates the immune system.
On March 30, Johnson & Johnson said human tests of its experimental vaccine will begin by September. “we have a candidate that has a high degree of probability of being successful against the covid-19 virus,” said Alex Gorsky, CEO of Johnson & Johnson, during an interview with NBC News’ Today. “”Literally within the next few days and weeks, we’re going to start ramping up production of these vaccines.”
DIOSynVax, a vaccine development company working out of the University of Cambridge, is trying to eschew the traditional pathways to vaccine creation with a new platform. The company’s approach uses computer modelling of the virus’s structure to determine weak spots in the SARS-CoV-2 DNA — places it can target to drive an immune reaction without causing any harm to the patient. “What we end up with is a mimic, a mirror image of part of the virus, but minus its bad parts,” said Jonathan Heeney, CEO and founder of DIOSynVax, in a statement. “What remains is just the magic bullet, essentially, to trigger the right type of immune response.”
Some research organizations, such as Boston Children’s Hospital, are examining different kinds of adjuvants that will help amplify the immune response. This approach, according to the Harvard Gazette, will be targeted more toward the elderly, who don’t respond as effectively when vaccinated. It’s hoped that by studying adjuvants to boost a vaccine, the elderly can be vaccinated with a mix of ingredients that would supercharge their immunity.
When will a vaccine be available?
Fauci, of the infectious diseases institute, posits that a vaccine is roughly a year and a half away, even though we’re likely to see human trials start within the next month or two. This, according to a 60 Minutes interview with Fauci in March, is a fast turnaround.
“The good news is we did it more quickly than we’ve ever done it,” Fauci told 60 Minutes. (Note: 60 Minutes and CNET share a common parent company, ViacomCBS.) “The sobering news is that it’s not ready for prime time, for what we’re going through now.”
Why does vaccine production take so long? There are many steps involved and a lot of regulatory hurdles to jump through.
“For any medicine to be sold it needs to go through the standard process of clinical trials including phase 1 [to] 3 trials,” said Bruce Thompson, dean of health at Swinburne University in Australia. “We need to ensure that the medicine is safe, will not do harm, and know how effective it is.”
Scientists can’t assume their vaccine design will just work — they have to test, test and test again. They have to recruit thousands of people to ensure the safety of a vaccine and how useful it will be. The process can be broken down into six phases:
- Vaccine design: Scientists study a pathogen and decide on how they will get the immune system to recognize it.
- Animal studies: A new vaccine is tested in animal models for disease to show that it works and has no extreme adverse effects.
- Clinical trials (phase I): These represent the first tests in human beings and test the safety, dose and side effects of a vaccine. These trials only enroll a small cohort of patients.
- Clinical trials (phase II): This is a deeper analysis of how the drug or vaccine actually works biologically. It involves a larger cohort of patients and assesses the physiological responses and interactions with the treatment. For instance, a coronavirus trial may assess if a vaccine stimulates the immune system in a certain way.
- Clinical trials (phase III): The final phase of trials sees an even greater amount of people tested over a long period of time.
- Regulatory approval: The final hurdle sees regulatory agencies, like the US Food and Drug Administration, the European Medicines Agency and Australia’s Therapeutic Goods Administration, take a look at the available evidence from experiments and trials and conclude whether a vaccine should be given the all-clear as a treatment option.
Traditionally, then, it could take a decade or more for a new vaccine to go from design to approval. In addition, once the regulatory processes have concluded a vaccine is safe, the drug companies have to send production into overdrive, so they can manufacture enough of the vaccine to increase immunity in the wider population.
With SARS-CoV-2, the process is being expedited in some instances. As STATnews reports, the vaccine in development by Moderna has moved from design straight into Phase I clinical trials of its mRNA vaccine, skipping tests in animal models. Those tests will take place at Seattle’s Kaiser Permanente Washington Health Institute, and patients are now being enrolled.
First US COVID-19 vaccine trials in humans
In the US, Moderna’s Phase I clinical trials began on March 16 in collaboration with NIAID, the US National Institutes of Health and KPWHRI. It is the first testing in humans of the mRNA vaccine and will look to enroll a total of 45 healthy adult volunteers aged between 18 and 55 years.
“This Phase 1 study, launched in record speed, is an important first step toward achieving that goal,” Fauci said in a statement.
Moderna’s approach, explained in the Vaccines section above, is particularly unique in its speed. Because the biotech company was already researching ways to tackle the coronavirus which causes Middle East respiratory syndrome, they were able to adapt their methodology and vaccine design for SARS-CoV-2. The experimental vaccine, dubbed mRNA-1273, contains genetic material from the spike protein present in SARS-CoV-2 embedded within a lipid nanoparticle.
Manufacturing costs were supported by the Coalition for the Epidemic Preparedness Innovations.
The trial will see patients receive two injections of the mRNA-1273 28 days apart. The 45 patients will be divided into three groups of 15 and given differing doses: Either 25 micrograms, 100 micrograms or 250 micrograms. Safety reviews will be performed after the first four patients receive the lowest and middle doses and again before all patients receive their shots. Another safety review of data will be performed before the 15 patients set to receive the highest dose are a injected.
Even if the vaccine is proven to be safe and shows promise in protecting against COVID-19, it could still be a year away — at least.
The US NIH has added a second site to the clinical trial of Moderna’s vaccine as of March 27. Emory University in Atlanta now be enrolling healthy adult volunteers aged between 18 and 55 into a Phase I trial. This will be an extension of the trial carried out in Seattle — and the ultimate goal is to enroll 45 participants across the two states.
You can visit NIAID’s website for all the information on the trial.
How do you treat COVID-19?
The best way to prevent illness is avoiding exposure. Those tips are below.
First: Antibiotics, medicine designed to fight bacteria, won’t work on SARS-CoV-2, a virus. If you’re infected, you will be asked to self-isolate, to prevent further spread of the disease, for 14 days. If symptoms escalate and you experience a shortness of breath, high fever and lethargy, you should seek medical care.
Treating cases of COVID-19 in the hospital is based on managing patient symptoms in the most appropriate way. For patients with severe disease adversely affecting the lungs, doctors place a tube into the airway so that they can be connected to ventilators — machines which help control breathing.
There are no specific treatments for COVID-19 as yet, though a number are in the works, including experimental antivirals, which can attack the virus, and existing drugs targeted at other viruses like HIV which have shown some promise in treating COVID-19.
Remdesivir
Remdesivir, an experimental antiviral made by biotech firm Gilead Sciences, has garnered a large part of the limelight. The drug has been used in the US, China and Italy, but only on a “compassionate basis” — essentially, this drug hasn’t received approval but can be used outside of a clinical trial on critically ill patients. Remdesivir isn’t specifically designed to destroy SARS-CoV-2. Instead, it works by knocking out a specific piece of machinery in the virus, known as “RNA polymerase,” which many viruses use to replicate. It has been shown in the past to be effective in human cells and mouse models.
Its effectiveness is still being debated, and much more rigorous study will be needed before this becomes a general treatment for SARS-CoV-2, if it does at all.
Gilead, the manufacturer was granted “orphan status” for remdesivir on March 23, which is usually reserved for development of drugs to diagnose or treat “rare diseases or conditions” that affect less than 200,000 people. The classification bestows a number of incentives on Gilead, including tax breaks and expensive fee waivers and is designed to hasten the development process. It also prevents other generic competitors from selling the drug. However, on March 25, Gilead asked the status to be rescinded after facing significant backlash from the public and presidential candidate, Bernie Sanders.
Favipiravir
Encouraging clinical trials in Wuhan and Shenzhen involving over 300 patients of the Japanese influenza drug favipiravir were reported by Chinese scientists in the Guardian on March 18. The drug appeared to shorten the course of the disease, with patients who were given the treatment clearing the virus after just four days, while those who did not took around 11 days.
The drug is manufactured by Fujifilm Toyama Chemical, but the company has declined to comment on the claims. Favipiravir, also known as Avigan, is an antiviral and is designed to target RNA viruses which include coronaviruses and influenza viruses. The drug is thought to disrupt a pathway which helps these viruses to replicate inside cells. According to the Guardian, a source within the Japanese health ministry suggests the drug is not effective in patients showing severe symptoms.
Other treatment options
An HIV medicine, Kaletra/Aluvia, has been used in China to treat COVID-19. According to a release by AbbVie, an Illinois-based pharmaceutical company, the treatment was provided as an experimental option for Chinese patients during “the early days” of fighting the virus. The company suggests it is collaborating with global health authorities including the Centers for Disease Control and Prevention and the World Health Organization.
On March 18, a randomized, controlled trial assessed the effectiveness of the HIV medicine. The results, published in the New England Journal of Medicine, show that adults with severe COVID-19 infections do not seem to benefit from the drug treatment and there was no clinical improvement versus standard care. The authors note additional studies should be undertaken because the treatment may reduce serious complications — such as acute kidney injury or secondary infections — if given at a certain stage of illness.
The trouble with chloroquine
A drug that has been used to treat malaria for around 70 years, chloroquine, has been floated as a potential treatment candidate. It appears to be able to block viruses from binding to human cells and getting inside them to replicate. It also stimulates the immune system. A letter to the editor in journal Nature on Feb. 4 showed chloroquine was effective in combating SARS-CoV-2. A Chinese study originating from Guangdong reports chloroquine improved patient outcomes and “might improve the success rate of treatment” and “shorten hospital stay.”
Tesla and SpaceX CEO Elon Musk and US President Donald Trump have both touted chloroquine as a potential treatment candidate. A more recent correspondence in the journal Nature, on March 18, suggests hydroxychloroquine — a less toxic derivative of the drug — is effective at inhibiting SARS-CoV-2 infection. That derivative is widely available to treat disease like rheumatoid arthritis and Chinese researchers have at least seven clinical trials in progress using hydroxychloroquine to treat infection.
Combining hydroxychloroquine with the antibiotic azithromycin has also been associated with positive patient outcomes. Doctors in Marseille, France, undertook a low-powered study with a small amount of patients (36) and suggested the combination treatment may be effective in reducing how much virus was found a particular part of the body. The study is being widely cited and even the president of the US suggested it could be a “game changer”. Whether this results in better clinical outcomes — ie. if patients recover more quickly — is still being debated.
“The results are disputed and the clinical trials inconclusive,” says Gaeten Burgio, a medical researcher at Australian National University. “To date there are no clear indications that chloroquine or hydroxychloroquine are a treatment option. Additional clinical trials will tell us whether hydroxychloroquine or chloroquine are viable options for COVID-19 treatments.”
Burgio advises against stockpiling hydroxychloroquine because the drug is critical for treating patients with the autoimmune condition Lupus.
The Food and Drug Administration commissioner, Stephen Hahn, discussed the investigations into chloroquine during a White House briefing on March 19. “That’s a drug that the president has directed us to take a closer look at as to whether an expanded use approach to that could be done to actually see if that benefits patients,” Hahn said. Trump announced the FDA approved chloroquine to be used on a “compassionate use” basis on March 19.
There’s another issue with chloroquine use, too.
Chloroquine phosphate, which is widely available, isn’t without its side effects, and health officials are warning against self-medicating. It can give you headaches, diarrhea, rashes, itching and muscle problems. It’s also used as an additive in fish tank cleaner. In rare cases, it seems to greatly affect the heart muscle and can result in abnormalities or heart failure. Health officials in Nigeria have reported cases of chloroquine poisoning and on March 23, a man in his 60s and his wife became critically ill after self-medicating with chloroquine phosphate, derived from fish tank cleaner. The man later died, and his wife was placed into critical care.
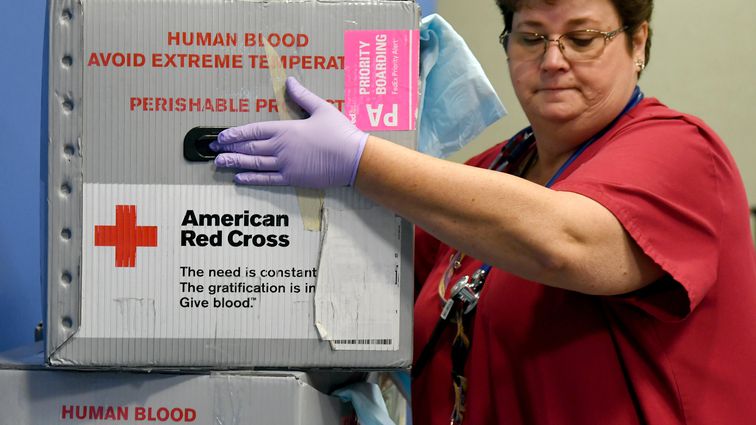
Convalescent plasma therapy
On March 24, the US FDA announced it would allow access to “convalescent plasma” for patients with serious or immediately life-threatening COVID-19 infections. This form of therapy sees a fraction of the blood from recovered COVID-19 patients infused into sick patients’ bodies.
As we’ve explained above, the immune system is the body’s defence force. When a virus invades, it sends out an army of cells, including white blood cells, to fight it off. Those cells release antibodies, which linger in the liquid portion of blood, known as “plasma.” If a patient survives COVID-19, they’re likely to have built up a huge stock of antibodies in their plasma. The idea is to take a portion of their stock and infuse it into seriously ill patients, hoping the antibodies will stimulate the patients’ own immune system to find and begin destroying the virus.
This isn’t the first time such a therapy would be used; previous outbreaks of SARS, MERS and the H1N1 influenza pandemic all saw the use of convalescent plasma to treat patients. In fact, the use of convalescent plasma stretches back to the 1918 influenza pandemic.
A report by Chinese scientists published in journal The Lancet Infectious Diseases in February suggested the treatment option could be viable in battling SARS-CoV-2 and anecdotal evidence from China has demonstrated some success, with 91 of 245 patients in a trial showing improvement, according to Xinhua.
In the US, New York Gov. Andrew Cuomo has announced New York doctors will begin to test convalescent plasma therapy in a trial starting in late March.
How you can protect yourself from coronavirus now?
It’s not a good idea to rely on a vaccine to stop the spread of coronavirus because that’s many months away. The best way to stop the spread, right now, is to continue practicing good personal hygiene and to limit interactions with others. “The best thing to do is the simple things like hand washing and hand sanitizing,” Thompson said.
This outbreak is unprecedented, and changing behaviors is absolutely critical to stopping the spread.
There are a huge number of resources available from the WHO on protecting yourself against infection. It’s clear the virus can spread from person to person, and transmission in communities has occurred across the world. Protection boils down to a few key things:
- Washing your hands: For 20 seconds and no less! You can get some handy handwashing tips here.
- Maintaining social distancing: Try to keep at least 3 feet (1m) away from anyone coughing or sneezing.
- Don’t touch your face, eyes or mouth: An incredibly difficult task, but this is how the virus initially gets into the body.
- Respiratory hygiene measures: Cough and sneeze into your elbow.
- If you’ve visited a location where COVID-19 is spreading, then self-isolate for 14 days.
For much more information, you can head to CNET’s guide
Originally published in March and constantly updated as new information becomes available.